USEFUL CONTACTS
| Name | Role | |
| Karis Ramsay | Clinical Learning and Development Lead for Primary Care | GPN Preceptorship Lead |
| Laura Halden | Clinical Chair- contact for Advanced Practice queries | glicb.pcwc@nhs.net |
| Hannah Gannon | Practice Education Facilitator – Primary Care Training Hub | Hannah.gannon2@nhs.net |
| Mashel Banks | GPN Preceptorship lead | Mashel.banks@nhs.net |
| Marie Altham | GPN Fellowship Lead | Marie.altham@nsh.net |
DISCOVERING A NURSING CAREER IN GENERAL PRACTICE
Nurses have an important role in delivering care within general practice. The 10-year plan aims to shift care from hospitals to community settings, presenting Nurses with career opportunities.
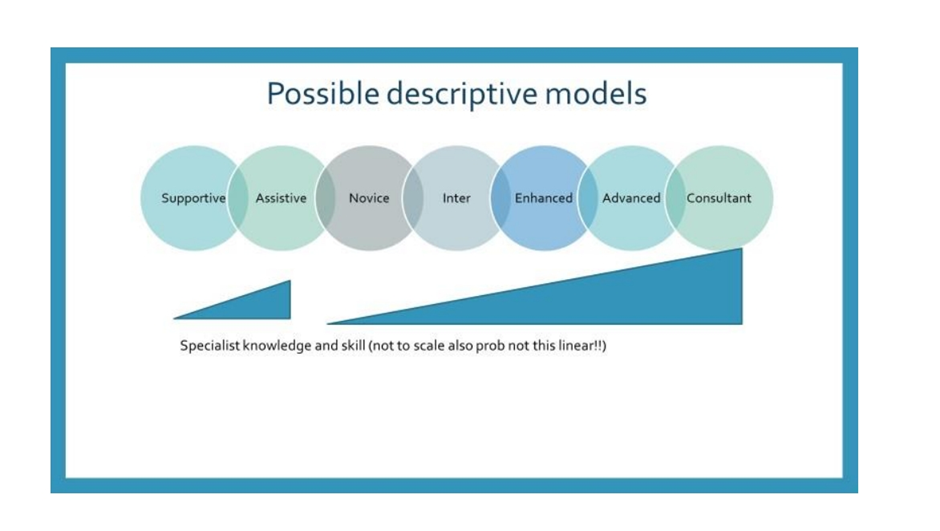
There are various levels within Practice Nursing that offer a structured career path for nurses to undertake numerous clinical activities, ranging from novice to competent. An example Practice Nursing Pathway can be accessed here.
General Practice Nurses provide care and treatment throughout the lifespan of the population they serve. The Primary Care and General Practice Nursing Career and Core Capabilities Framework was developed to set standards and define the scope of practice for nurses within General Practice.
The framework includes:
Career framework – summarising 6 career levels for nurses within Primary Care
Core Capabilities – outlining the knowledge, skills, and behaviours at different practice levels.
All levels of nurses in Primary Care should operate within the framework to ensure workforce readiness for the future. Utilisation of the framework can be found here. Designing the workforce for the future, nurses and their employers can utilise the framework to plan, educate and inform career development.
COURSES FOR NURSES WANTING TO START A CAREER IN GENERAL PRACTICE
- Fully funded module, level6/7, 20 credits and a mixture of online/blended learning
- Increase awareness of Primary Care and general Practice
- Covers knowledge, skill and understanding of a primary care environment
Delivers through the following universities:
PRECEPTORSHIP PROGRAMME FOR ALL NEWLY QUALIFIED AND TRANSITIONING RNs/RNAs
New nurses in primary care can join a preceptorship programme tailored for them. This programme supports newly qualified Registered Nurses, Nursing Associates and Nurses transitioning from secondary/community/social care settings. A period of preceptorship allows new nurses to become familiar with their new clinical environment. The programme offers time for our new nurses to reflect on clinical practice with a PROFESSIONAL NURSE ADVOCATE, which allows them to develop their practice, and provide high-quality and safe care to the population they serve.
Please contact Mashel Banks (mashel.banks@nhs.net) for further information
Further information on our Preceptorship programme can be found HERE
JOB VACANCIES
Candidates can contact Karis.ramsay1@nhs.net to discuss current job vacancies advertised internally and vacancies advertised through NHS jobs for further advice.
Employers can contact karis.ramsay1@nhs.net to discuss vacancies. Support can be given regarding advertising and job descriptions. All vacancies can be advertised via the nursing forum; PCN newsletters; Nursing Newsletters; University of Gloucestershire career boards
The network contract DES for 2025/2026 now allows Primary Care to hire General Practice Nurses through the Additional Roles Reimbursement Scheme (ARRS) or directly by surgeries. Information regarding the DES can be found here.
INDUCTION SUPPORT
A link to the Primary Care Nurse induction book can be accessed here.
There are also bimonthly inductions to primary care supported by the Primary care workforce team – further details can be found here.
CONTINUING PROFESSIONAL DEVELOPMENT (CPD) FUNDING
Government funding has been made available to support Allied Health professionals (AHPs), Nurses and Midwives with Continuing Professional Development across the UK. The funding is there to help you build upon existing skills that are vital to the services and communities we support. Funded CPD should be specifically linked to your personal professional requirements, as well as system and population health priorities.
HOW TO ACCESS CPD FUNDING
Each PCN has an appointed Education Lead responsible for annually submitting CPD requirements for AHP/Nursing. This ensures that the necessary funding is allocated according to professional needs. Consequently, CPD funds are maintained within your PCN and should be requested from your Education Lead.
NURSES SUPPORT
Working in the Health Sector can be an incredibly rewarding job; but we all know that sometimes. The fast-paced environment, workloads and pressure that make it exciting can take its toll. Everyone can need some extra support or a place to turn to from time to time, whether it’s career advice or a more difficult subject, a signpost or a friendly ear can go a long way to solving the problem.
The Wellbeing line

Unlocking confidential mental health and wellbeing support for anyone working in health and social care in Gloucestershire.
Zero Suicide alliance
The Zero Suicide Alliance is a collaborative of National Health Service trusts, businesses and individuals who are all committed to suicide prevention in the UK and beyond. The alliance is ultimately concerned with improving support for people contemplating suicide by raising awareness of and promoting FREE suicide prevention training which is accessible to all. The aims of this training are to: enable people to identify when someone is presenting with suicidal thoughts/behaviour, to be able to speak out in a supportive manner, and to empower them to signpost the individual to the correct services or support.
To access their services and FREE training Click Here >
“Cavell Nurses” Trust
This Trust is the charity that supports UK nurses, midwives, and healthcare assistants, both working and retired, when they’re suffering personal or financial hardship often due to illness, disability, older age, and domestic abuse. From simple, essential support like money to repair a broken cooker, to vital life changing aid like helping a family flee their home due to domestic abuse, Cavell Nurses’ Trust is here to help.
Individual Coaching: sarah.rogers11@nhs.net
NHSE Coaching: https://www.england.nhs.uk/supporting-our-nhs-people/wellbeing-support-options/looking-after-you-too/
Professional Nurse Advocacy: (Wednesday only) mashel.banks@nhs.net
Royal College of Nursing (RCN – Managing Stress): Managing stress | Royal College of Nursing
NURSE LEADERSHIP
Whatever level we nurse at we are leaders, developing these skills and qualities can help us to feel confident in our roles. See below for resources available.
A toolkit has been developed in Yorkshire and across the Midlands in collaboration with a WTE team to support and assist General Practice Nurses (GPNs) and lead GPNs who are providing advice and support.
The Leadership Toolkit can be accessed here.
For Short Courses:
PROFESSIONAL NURSE ADVOCATE
PNA training provides those on the programme with skills to facilitate restorative supervision to their colleagues and teams, in nursing and beyond. A version of this programme exists already for maternity colleagues, where outcomes point to improved staff wellbeing and retention, alongside improved patient outcomes. The training equips them to listen and to understand challenges and demands of fellow colleagues, and to lead support and deliver quality improvement initiatives in response.
Please contact Sarah – sarah.rogers11@nhs.net for further support if you would like to undertake this course.
STUDENT PLACEMENTS
We support and encourage practices to have nursing students. This helps inspire the next generation of nurses to consider Primary Care as a viable career option and dispels myths about it not being a first destination career choice. To become a supervisor/assessor see tab.
NURSE ON TOUR supports Students Placements and is a population health initiative which meets student nurse placement demand through an innovative approach to healthcare.
Student Nurses are given the opportunity to have a day in the life of a General Practice Nurse whilst offering NHS checks to patients under supervision, either on a health bus or within a community setting. If your surgery or community group would like to be involved in this scheme please contact: Karis.Ramsay1@nhs.net ; Chloe.fletcher4@nhs.net or sarah.rogers11@nhs.net

